Severe malnutrition in infants aged <6 months—Outcomes and risk factors
Table Of Contents
Chapter ONE
1.1 Introduction1.2 Background of Study
1.3 Problem Statement
1.4 Objective of Study
1.5 Limitation of Study
1.6 Scope of Study
1.7 Significance of Study
1.8 Structure of the Research
1.9 Definition of Terms
Chapter TWO
2.1 Overview of Severe Malnutrition2.2 Global Prevalence of Severe Malnutrition
2.3 Causes of Severe Malnutrition
2.4 Effects of Severe Malnutrition
2.5 Diagnosis and Treatment of Severe Malnutrition
2.6 Nutritional Interventions for Severe Malnutrition
2.7 Psychosocial Impact of Severe Malnutrition
2.8 Economic Burden of Severe Malnutrition
2.9 Public Health Policies Addressing Severe Malnutrition
2.10 Emerging Trends in Severe Malnutrition Research
Chapter THREE
3.1 Research Design and Methodology3.2 Selection of Sample Population
3.3 Data Collection Methods
3.4 Data Analysis Techniques
3.5 Ethical Considerations
3.6 Validity and Reliability of Data
3.7 Research Limitations
3.8 Research Assumptions
Chapter FOUR
4.1 Overview of Research Findings4.2 Demographic Characteristics of Study Participants
4.3 Prevalence of Severe Malnutrition in Infants
4.4 Risk Factors Associated with Severe Malnutrition
4.5 Impact of Nutritional Interventions
4.6 Comparison with Existing Literature
4.7 Recommendations for Policy and Practice
4.8 Future Research Directions
Chapter FIVE
5.1 Summary of Findings5.2 Conclusion
5.3 Implications for Public Health
5.4 Recommendations for Further Action
5.5 Contribution to the Field of Severe Malnutrition Research
Project Abstract
Abstract
Severe acute malnutrition (SAM) affects ~4 million infants under 6 months (u6m) worldwide, but evidence underpinning their care is “very low” quality. To inform future research and policy, the objectives of our study were to identify risk factors for infant u6m SAM and describe the clinical and anthropometric outcomes of treatment with current management strategies. We conducted a prospective cohort study in infants u6m in Barisal district, Bangladesh. One group of 77 infants had SAM (weightâ€forâ€length Zâ€score [WLZ] <−3 and/or bipedal oedema); 77 others were “nonâ€SAM” (WLZ ≥−2 to <+2, no oedema, midâ€upperâ€arm circumference ≥125 mm). All were enrolled at 4–8 weeks of age and followed up at 6 months. Maternal education and satisfaction with breastfeeding were among factors associated with SAM. Duration of exclusive breastfeeding was shorter at enrolment (3·9 ± 2.1 vs. 5.7 ± 2.2 weeks, P < 0.0001) and at age 6 months (13.2 ± 8.9 vs. 17.4 ± 7.9 weeks; P = 0.003) among SAM infants. Despite referral, only 13 (17%) reported for inpatient care, and at 6 months, 18 (23%) infants with SAM still had SAM, and 3 (3.9%) died. In the nonâ€SAM group, one child developed SAM, and none died. We conclude that current treatment strategies have limited practical effectiveness poor uptake of inpatient referral being the main reason. World Health Organization recommendations and other intervention strategies of outpatientâ€focused care for malnourished but clinically stable infants u6m need to be tested. Breastfeeding support is likely central to future treatment strategies but may be insufficient alone. Better case definitions of nutritionally atâ€risk infants are also needed.
Project Overview
1. INTRODUCTION
Undernutrition is responsible for 45% of all underâ€5 child deaths (Black et al., 2013) and affects progress towards numerous Sustainable Development Goals (Greenslade, 2015). Target 2.2 of Sustainable Development Goals 2 (Zero Hunger) aims to “By 2030, end all forms of malnutrition, including stunting and wasting in children under 5 years of age” (Sustainable Development Goals, 2015).
Over the last decade, the treatment of malnourished children aged 6–59 months has been revolutionized by a publicâ€health focused model of care, “Community Management of Acute Malnutrition” (CMAM; Bhutta et al., 2017; Trehan & Manary, 2015). Yet, despite some 4 million infants worldwide being severely wasted (Kerac et al., 2011) with a higher risk of death than older children (Grijalvaâ€Eternod et al., 2017), malnourished infants aged under 6 months (u6m) have long been neglected (Kerac, Mwangome, McGrath, Haider, & Berkley, 2015). This problem was most recently highlighted in the updated World Health Organization (WHO, 2013) guidelines on “The Management of Severe Acute Malnutrition (SAM) in Infants and Children.” Although this document includes a chapter on infants u6m (for the first time), “very low quality” underlying evidence is acknowledged (WHO, 2013). Others, including 64 national and international experts who contributed to a 2015 Child Health and Nutrition Research Initiative research prioritization exercise, have also highlighted major evidence gaps around this vulnerable patient group (Kerac et al., 2015). Especially lacking is evidence for the potential safety and effectiveness of homeâ€based treatment of clinically stable infants u6m with SAM (Kerac et al., 2015).
Bangladesh guidelines are typical of almost all current national SAM guidelines (Kerac et al., 2017) in that they only describe inpatient care (IPHN/DGHS/MoHFW/PRB, 2008). As in the early days of CMAM for older children, a shift to outpatient/community care is a significant paradigm change that is politically and programmatically sensitive (Kerac et al., 2015).
To move forward, data on potentially modifiable risk factors and outcomes using current inpatientâ€only treatments are needed. This is vital need for researchers, policymakers, and programme managers to design and test better future interventions. Our goal was to address these research gaps. Our first aim was to identify risk factors associated with infant u6m SAM and, second, to describe the clinical and anthropometric outcomes of treatment using current management strategies.
2. PARTICIPANTS AND METHODS
2.1. Study design and participants
We conducted a prospective cohort study. This involved two groups, each consisting of 77 infants aged 4–8 weeks (the age when future interventions to treat infant u6m SAM will be anticipated to begin; Mwangome, Fegan, Fulford, Prentice, & Berkley, 2012). One group comprised infants with SAM as defined by current WHO guidelines: weightâ€forâ€length Zâ€score (WLZ) <−3 and/or bilateral nutritional oedema (WHO, 2013); the other comprised age†and sexâ€matched infants who were not severely malnourished (nonâ€SAM) defined as WLZ ≥−2 to <2 and midâ€upperâ€arm circumference (MUAC) ≥125 mm. Exclusions were infants from twin/multiple pregnancies and those with obvious congenital anomalies that could affect feeding (e.g., cleft lip or palate).
Ethical approval was obtained from the Institutional Review Board of International Centre for Diarrhoeal Disease Research, Bangladesh (icddr, b; PR14112). Written informed consent was obtained from the infants' parents or legal guardians. The study is registered with the ISRCTN trial registry: http://www.isrctn.com/ISRCTN12494235.
2.2. Variables
The primary outcome was the proportion of infants who died or who had SAM (defined as per WHO criteria as WLZ <−3 and/or MUAC <115 mm and/or oedema) at age 6 months (180 completed days). Key secondary outcomes were changes in and absolute values of weightâ€forâ€length zâ€score (WLZ), weightâ€forâ€age zâ€score (WAZ), and lengthâ€forâ€age zâ€score (LAZ).
Maternal mental health status was assessed using the WHO Self Reporting Questionnaire 20 (SRQ 20; WHO, 1994). Mothers who had a high total score (≥13) or who answered “Yes” to question no. 17 (“Has the thought of ending your life been on your mind?”) were referred to the outpatient psychiatry department at the nearby Sherâ€eâ€Bangla Medical College Hospital, Barisal, for appropriate management.
At cohort end line (age ≥ 6 months), infants' vital status, anthropometry, and dietary history were repeated.
2.3. Data collection procedures
2.3.1. Anthropometry
Anthropometric assessments were performed following the standard procedures (SMART, 2017). Length was measured using a portable length measuring board to 0.1 cm (Shorrboard, Weigh and Measure, LLC, Maryland, USA). Weight was measured using a digital scale accurate to 5 g (Digital Kinlee, Taiwan). MUAC was measured with UNICEF measuring tapes to 1 mm. Infants' reported birth date was verified against a birth certificate or immunization card whenever possible. Oedema was assessed by pressing the upper side of both feet by pressing for 3 s. Maternal anthropometry was measured only for the prospective cohort study at enrolment: Weight was measured with a scale accurate to 100 g and height by a height board graduated to the nearest 0.1 cm. Regular checks of weighing scale and length/height board calibration were carried out with a known weight and length, respectively.
2.3.2. Data collection procedures
SAM “case” infants were identified by household visits. Age†and sexâ€matched controls were also selected by household visits in Barisal district of Bangladesh. Study participants were identified by the set criteria as mentioned above.
For both parts of the study, data were collected electronically: This enabled immediate validation of key variables. Supervisors also checked incoming data daily for completeness and consistency.
2.4. Sample size estimation and statistical analysis
Sample size for the prospective cohort study was estimated for comparing outcomes in the exposed group (SAM) and unexposed group (nonâ€SAM) assuming that 25% of the participants in the SAM group would have SAM at 6 months of age and 6.3% of the participants in the nonâ€SAM group would have SAM at the same time point (the prevalence of SAM in infants u6m in Bangladesh during designing the survey; NIPORT, Mitra, & ICF, 2013). With 5% level of significance and 80% power, 77 infants were required per group, assuming approximately 25% loss to followâ€up at the end of 6 months. The following formula was used for sample size estimation: [(pA1−pA/κ+pB1−pB]z1−α/2+z1−β/pA−pB2 [available at http://powerandsamplesize.com/Calculators/Compareâ€2â€Proportions/2â€Sampleâ€Equality].
Anthropometric zâ€scores (standard deviation scores) were calculated from raw age, sex, length, and weight data using WHO, 2006 growth standards and WHO Anthro software (WHO, 2006). LAZs and WLZs were calculated for infants who were ≥45 cm long (WHO 2005). WAZs were calculated for all infants. Those with extreme values were excluded from analysis following standard WHO “cleaning rules,” WAZ <−6.0 or WAZ >+5.0, LAZ <−6.0 or LAZ >+6.0, and WLZ <−5.0 or WLZ >+5.0 SD (Crowe, Seal, Grijalvaâ€Eternod, & Kerac, 2014).
Potential explanatory variables were grouped under household characteristics, maternal characteristics, and infant characteristics. Differences between groups were tested using chiâ€squared tests for proportions, Student's t test for normally distributed continuous variables, and Mann–Whitney U test for skewed continuous variables. Multivariable logistic regression was performed for adjustments of different variables and potential risk factors for SAM. Multiple linear regression analysis was also used to adjust the potentially confounding variables when different variables were compared for test of significance. The potential confounders were considered to be the age of the infants at the time of enrolment, monthly income, and maternal education. All the tests were considered as significant at P < 0.05. Statistical analysis was done with the Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.).
3. RESULTS
3.1. Sociodemographic characteristics
Infants in the SAM group were over a week younger at enrolment than those in the nonâ€SAM group (5.1 ± 1.2 weeks vs. 6.5 ± 1.2 weeks, P = 0.001). Median household monthly income was significantly lower (P = 0.007) in SAM group, and mothers were less educated (P = 0.005) also. Fewer households in the SAM group had electricity (P = 0.013). Other reported sociodemographic characteristics were comparable between groups (Table 1).
Table 1
Sociodemographic characteristics of the study participants
Note. All tests of significance are Pearson chiâ€square test, unless mentioned. Level of significance <0.05. SAM: severe acute malnutrition.
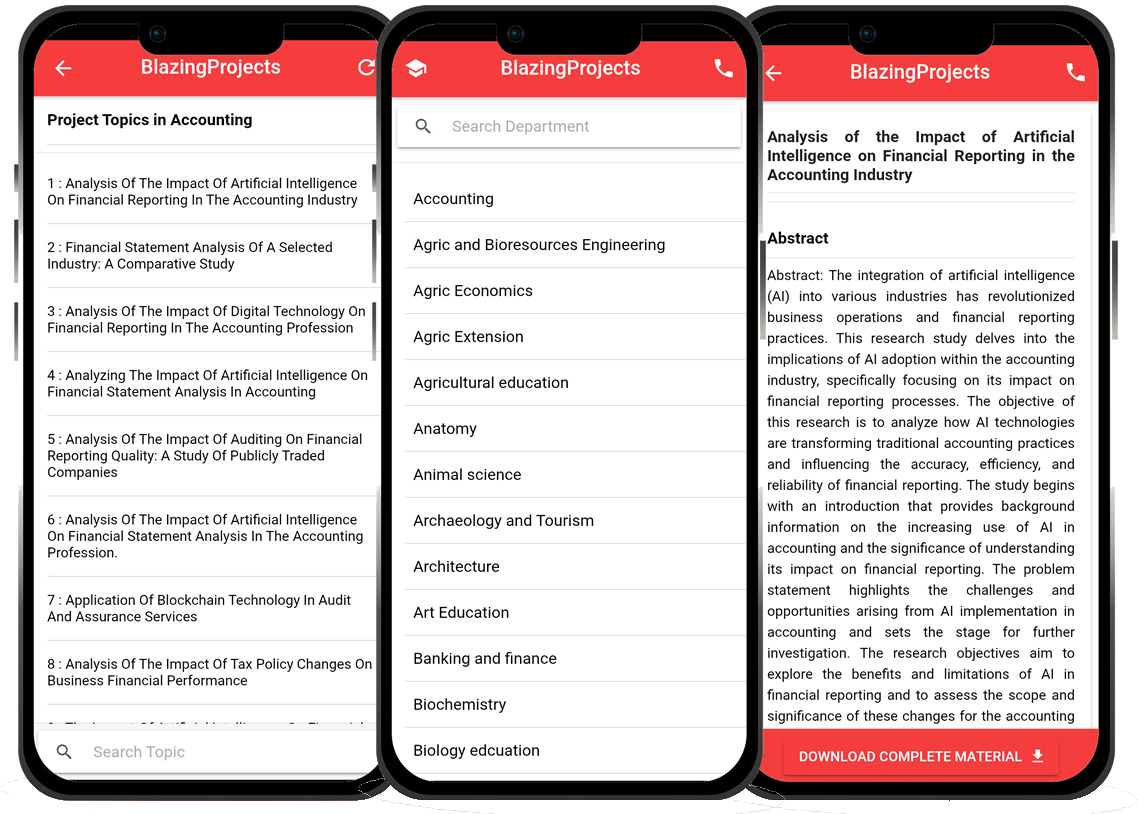
Blazingprojects Mobile App
📚 Over 50,000 Project Materials
📱 100% Offline: No internet needed
📝 Over 98 Departments
🔍 Software coding and Machine construction
🎓 Postgraduate/Undergraduate Research works
📥 Instant Whatsapp/Email Delivery
Related Research
Utilizing Telemedicine for Pediatric Healthcare in Remote Areas...
"Utilizing Telemedicine for Pediatric Healthcare in Remote Areas"...
Use of Telemedicine for Pediatric Care in Remote Areas...
The project topic, "Use of Telemedicine for Pediatric Care in Remote Areas," focuses on exploring the application of telemedicine to enhance pediatric...
Assessment of the Impact of Telemedicine on Pediatric Care in Rural Communities...
The project titled "Assessment of the Impact of Telemedicine on Pediatric Care in Rural Communities" aims to investigate the effects of telemedicine o...
Use of Telemedicine in Pediatric Care: Impact on Patient Outcomes and Healthcare Acc...
The project topic, "Use of Telemedicine in Pediatric Care: Impact on Patient Outcomes and Healthcare Accessibility," focuses on the integration of tel...
The Impact of Virtual Reality-Based Therapy on Pain Management in Pediatric Patients...
Research Overview: Virtual Reality (VR) technology has gained recognition for its potential in transforming healthcare practices, particularly in the field of ...
The Impact of Telemedicine on Pediatric Care Delivery and Parental Satisfaction...
The project topic "The Impact of Telemedicine on Pediatric Care Delivery and Parental Satisfaction" delves into the intersection of modern technology,...
The Impact of Telemedicine on Pediatric Healthcare Outcomes...
The use of telemedicine in pediatric healthcare has been gaining momentum in recent years, offering a promising avenue to enhance healthcare outcomes for childr...
Implementation and Evaluation of Telemedicine in Pediatric Care...
The project topic, "Implementation and Evaluation of Telemedicine in Pediatric Care," focuses on the integration of telemedicine into the field of ped...
Effectiveness of Telemedicine in Improving Access to Pediatric Care in Rural Areas...
The project topic "Effectiveness of Telemedicine in Improving Access to Pediatric Care in Rural Areas" aims to investigate the impact of telemedicine ...